Analgesia
Pain is one of the most common reasons you'll be paged to review a patient, so having a good understanding of analgesia is important to feeling confident in responding to these calls.

High-Yield Tips
- Be conservative! You can always give more analgesia but you can't take it out of the patient.
- Be particularly cautious in: elderly patients, patients with renal impairment, patients with hepatic impairment, those with respiratory issues.
- Main adverse effects of opioids include: respiratory depression, sedation, constipation, nausea.
- Ensure the patient is well-monitored after any opioid administration.
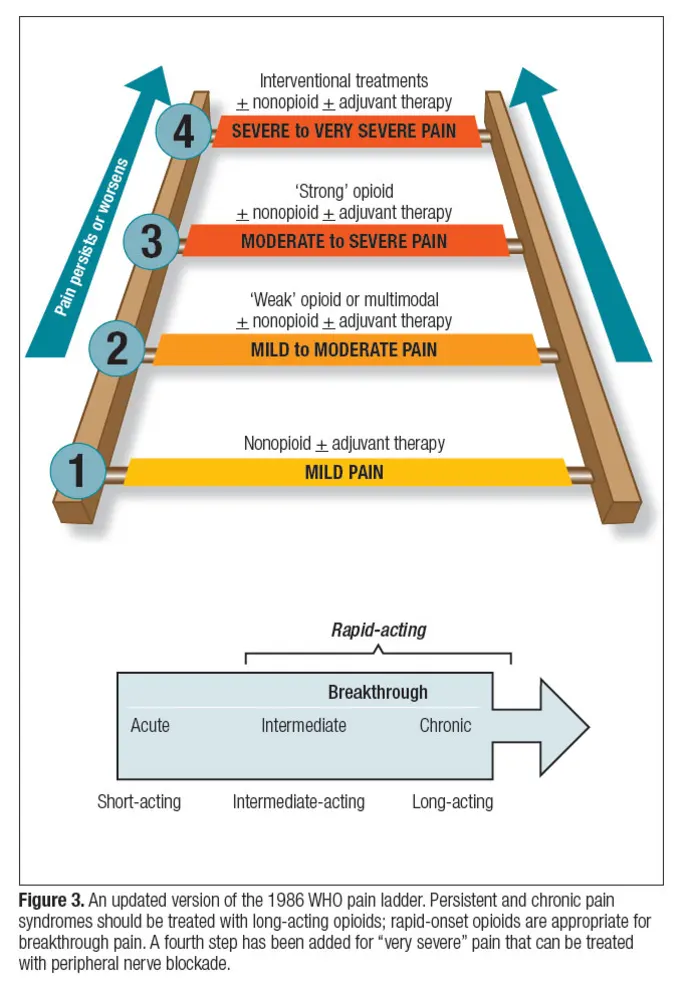
- Use the WHO Pain Ladder as a framework for what level of analgesia may be required for the pain that the patient is experiencing.
WHO Pain Ladder
Principles
- Start at the level most appropriate for the patient
- e.g. acute pain in ED → can start at level 2
- e.g. chronic pain on the wards → can start at level 1 (or non-pharmacological)
- Re-evaluate patient’s response to therapy
- Titrate dose and medication to patient’s response
- Aim to have patient’s pain managed on the lowest step possible at the lowest dose
- Aim for realistic goals
- i.e. goal isn’t to remove pain entirely, but remove it enough that rehab and ADLs can be performed
- Choose right dosing regimen
- e.g. better to have regular paracetamol +/- NSAIDs, rather than PRN
- Consider whether regular opioids are required or if only PRNs are required for acute flares of pain (”breakthrough” pain)
- Choose the right drug
- Consider what type of pain is present (e.g. neuropathic vs somatic), organ function (e.g. renal or hepatic impairment), response to prior therapy (e.g. allergies), duration of action required (e.g. short- vs long-acting)
Steps
Non-Pharmacological Therapies
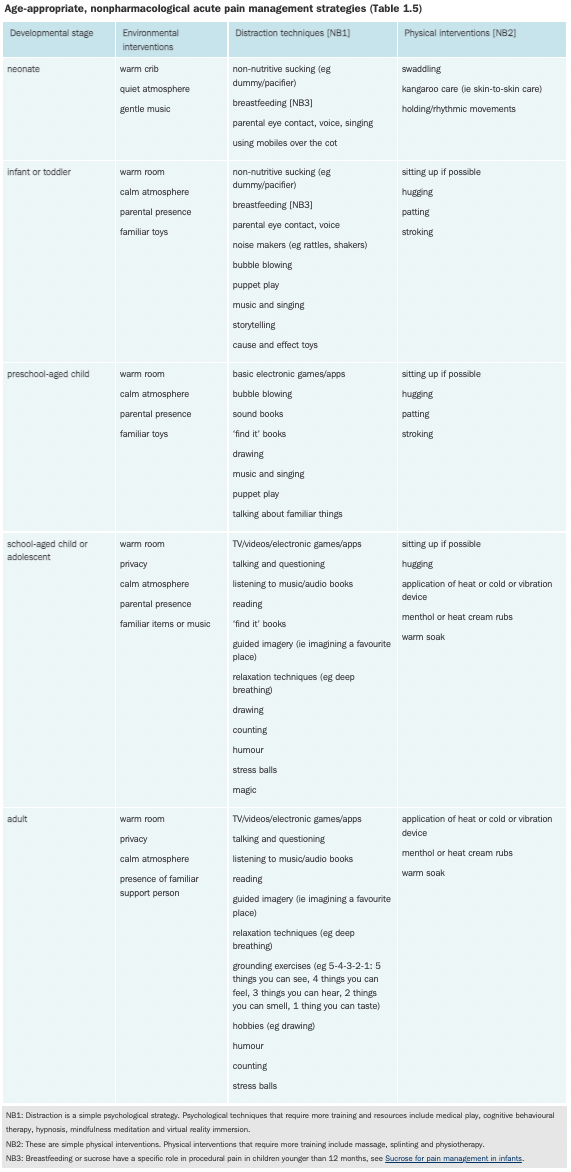
- Note: in a patient with a fracture or dislocation, splinting/sling or reduction is another useful non-pharmacological pain management strategy
Pharmacological Therapies
Non-opioids
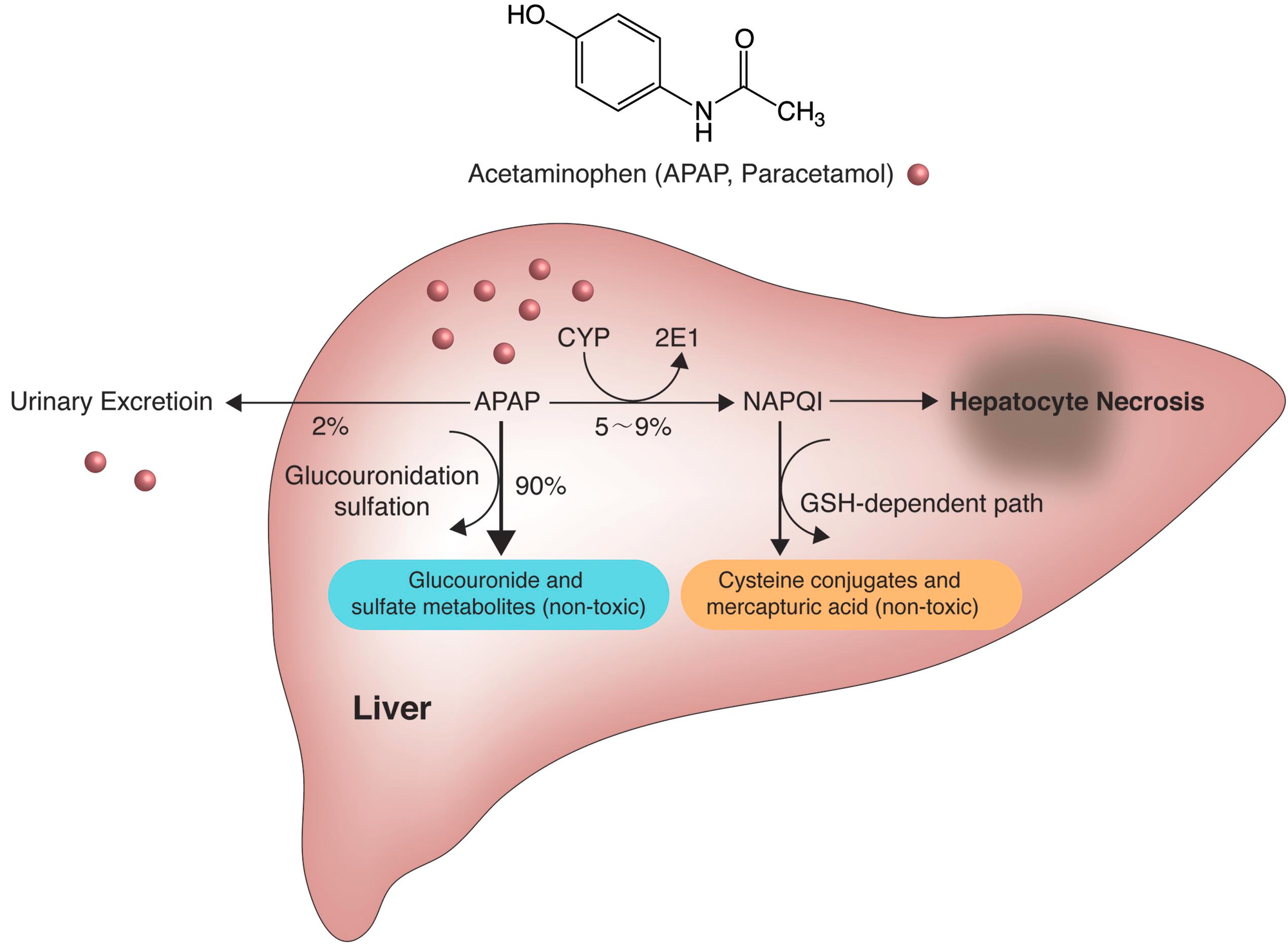
Paracetamol
- In addition to analgesic effects, also provides anti-pyretic effects
- MoA: ?
- Route of administration: PO, IV, PR
- PO onset of action: 20-30 mins
- Dose: 1g QID or PRN q4-6h
- Max dose: 4g in 24h
- Considerations:
- Dose adjustment in: liver failure, low body weight (< 50kg), older age
NSAIDs
- In addition to analgesic effects, also provides anti-inflammatory, antiplatelet and anti-pyretic effects
- MoA: COX enzyme inhibition
- Classification:
- Non-selective COX inhibitors (most) e.g. ibuprofen, aspirin, diclofenac, naproxen, indomethacin
- Preferential COX-2 inhibitors e.g. meloxicam
- Selective COX-2 inhibitors e.g. parecoxib, celecoxib
- No platelet inhibition thus ↓ bleeding risk compared to other NSAIDs
- Also ↓ GI toxicity compared to non-selective COX-inhibitors
- Route of administration: PO, IM, IV, PR, topical
- Dose (ibuprofen): 400mg PO TDS or 200-400mg PO PRN
- Max dose: 1200mg in 24h
- Dose (celecoxib): 100-200mg PO BD
- Max dose: 400mg in 24h
- Considerations:
- Avoid in: elderly (> 75y), renal disease, use of ARBs/ACE-Is, peptic ulcer disease, cardiovascular disease, coagulation disorders, severe hepatic impairment, surgery
- If patient is in pain, chart as regular as nursing staff may not give if it's PRN
- Risks:
- Renal impairment (in dehydrated patients, those already on drugs that reduce GFR, post-surgical patients)
- ↑ bleeding risk
- Peptic ulcer disease or GI bleed
- ↑ risk of cardiovascular events (in patients with pre-existing CVD)
- NSAID-induced bronchospasm (in asthmatics)
Opioids
- All patients respond differently to different opioid drugs.
- Major problems of opioids include: respiratory depression, sedation, nausea (acutely), constipation, dependence, hypotension
- Think about dose adjustment in certain patient populations: elderly, low body weight, renal impairment, respiratory issues
- Ensure patients are being monitored regularly with pulse oximetry, BP measurements and nursing staff review
Weak Opioids
Codeine
- MoA: very weak μ-receptor agonist
- Analgesic action depends on metabolism (~10% metabolised to morphine)
- Route of administration: PO
- Dose: 30-60mg q4h
- Max dose: 240mg in 24h
- Duration of action: ~4h
- Considerations:
- Interethnic differences in the variant CYP 2D6 alleles required for metabolism (ultrametabolisers vs poor metabolisers)
- GI effects → always chart with aperients
Tramadol
- MoA (tramadol itself and its M1 metabolite): weak μ-receptor agonist + serotonin and noradrenaline reuptake inhibitor
- Route of administration: PO, IM
- PO formulations: immediate-release and slow-release
- Dose: 50-100mg PRN q4-6h
- Max dose: 400mg in 24h
- PO onset of action: ~1h post-administration
- Considerations:
- Dose adjustment in: elderly, renal impairment, severe hepatic impairment
- Less respiratory depression and GI effects than other opioids
- Risks:
- Serotonin toxicity
Strong Opioids
Oxycodone
- Semi-synthetic opioid
- Good oral bioavailability with fast onset of action
- Route of administration: PO, IV, SC
- PO formulations: immediate release tablet (Endone), controlled release tablet (OxyContin), immediate release cap (OxyNorm), tablet with naloxone (Targin)
- The addition of naloxone (in Targin) is (theoretically) to ↓ constipation + ↓ diversion
- As naloxone is metabolised by the liver, naloxone-based therapies are contraindicated in moderate to severe hepatic impairment
- PO formulations: immediate release tablet (Endone), controlled release tablet (OxyContin), immediate release cap (OxyNorm), tablet with naloxone (Targin)
- PO dose: 2.5-15mg q4h + titrate to effect
- Duration of action: 3-6h (immediate release), 12h (controlled release)
- Considerations:
- Dose adjustment in: elderly, renal impairment
Morphine
- Prototypical opiate → used as reference for all others
- Generally provides good 'quality' of analgesia
- Route of administration: PO, SC, IV
- PO formulations: tablet (Sevredol), liquid (Ordine), controlled release tablet (MS Contin), controlled release cap (Kapanol)
- Poorly lipid soluble:
- Onset of action: ~5 mins
- Peak effect: ~20 mins
- Dose (age-dependent → refer to AMH): ~0.1-0.15mg/kg for most patients
- Duration of action: ~3-4h
- Metabolised into M3G (little analgesic effect, neuroexcitatory effects → myoclonus, allodynia, seizures) and M6G (potent analgesic effect)
- Considerations:
- Nausea and sedation particularly problematic
- Available on the ward in 10mg/1mL ampoules
- Volume of distribution is important for initial dosing
- Clearance affects duration of action → important for repeated dosing and infusions. Clearance is affected in renal impairment → accumulation of metabolites.
💡
It is safe to use morphine in the acute setting for patients with renal failure.
Fentanyl
- Synthetic opioid
- Extremely potent
- Highly lipophilic:
- Onset of effect: 2-3 mins
- Peak effect: ~3-5 mins
- Duration of effect: 20-40 mins following a single dose
- No active metabolites → does not accumulate in renal dysfunction
- Route of administration: IM, SC, IV, TD, IN
- Dose: ~1-3 mcg/kg q4h for most adults
- Considerations
- Unpredictable IM/SC/TD absorption → only IV administration suitable acutely
- Present in 100mcg/2mL and 500mcg/10mL ampoules
- Dose reduction from age > 40 (check AMH)
- ↑ risk of serotonin toxicity (avoid with MAOI)
Hydromorphone
- Only indicated for patients intolerant of morphine and oxycodone
- Requires specialist supervision
- Dose reduction in renal and hepatic impairment
- About 5-6x more potent than morphine
IV Administration of Opioids
- Verify:
- Patient details, drug, route
- Allergy status of patient
- Patency of cannula
- Monitoring, oxygen, emergency plan, equipment
- Steps:
- Disinfect access port with alcohol wipe and allow to dry
- Administer initial dose and flush line to ensure it reaches the patient
- Monitor vital signs and response
- Do not administer more until magnitude of response apparent
- If more required, flush after each incremental dose
Sedation Score
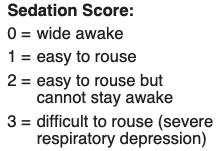
- Aim to keep sedation score < 2.
- Score ≥ 2 suggests early respiratory depression → no further opioids should be given.
- If a patient is still in pain, but has a sedation score of ≥ 2, consider referral to Acute Pain Service (APS).
Adjuvant Therapies
Ketamine
TBA
Local & Regional Anaesthesia as Analgesia
- Contact the APS for this → only indicated after other initial treatments have been initiated.
Other Tips
- Patient Controlled Analgesia (PCAs) can only be initiated by the APS.
- In most cases, pre-surgical patients who are Nil By Mouth (NBM) can still be given oral medications up to 2h prior to surgery.
Related Articles
Resources
- Lecture given by Dr Rebekah Potter
- Practical Pain Management: The WHO Pain Ladder: Do We Need Another Step?
- AMH
- Australian Prescriber: How to adjust drug doses in chronic kidney disease
- Australian Prescriber: Prescribing in renal disease
- Opioid Metabolism